Did you know? As many as 15%[1] of couples in Singapore are unable to conceive within a year of trying for a child. Unsurprisingly, the number of Singaporean parents-to-be opting for IVF continues to climb steadily – from 2013 to 2017 alone, the number of IVF cases jumped from 5,500 to 7,700.
Getting pregnant is not as easy as most people think, and artificial conception is not able to promise a child; even if success is had, it can often take copious tries, financial sacrifices, and umpteen emotional rollercoaster rides.
If you’re part of the population that’s desperately trying to conceive, you are not alone. And if you and your partner are considering IVF, you might want to think about going for IUI (intrauterine inseminations) first.
In this article, we cover why IUI could be a great first option for many couples. Additionally, is IUI or IVF the better treatment option for you and your partner?
What are the fertility treatments available in Singapore?
According to SingHealth, more and more couples are pursuing options such as making lifestyle changes, bettering their diets; reducing stress; opting for Traditional Chinese Medicine (TCM), or even going for fertility wellness staycation in their attempts to conceive.
Apart from that, fertility treatments in the form of medications are also available for couples hoping to conceive and are a comparatively inexpensive solution.
For example, Clomiphene, which is used by women who are unable to become pregnant, works by altering one’s hormonal balance, causing ovulation to occur and preparing the body for conception. We call this ovulation induction.
The first step that every couple having trouble conceiving should take is to consult a trusted gynaecologist. Factors such as age, PCOS, high stress, and other underlying medical conditions can severely affect fertility, and your doctor will be able to help ascertain if you should go down the route of IUI or IVF.
Key Decisions In IUI and IVF Treatment in Singapore
Whether you choose IUI or IVF, many key decisions have to be made by you and your gynaecologist. Let’s take a look at some of them:
| During IVF, your eggs are retrieved through a quick 10-minute procedure, combined with sperm, and then back into your uterus. | IUI | IVF |
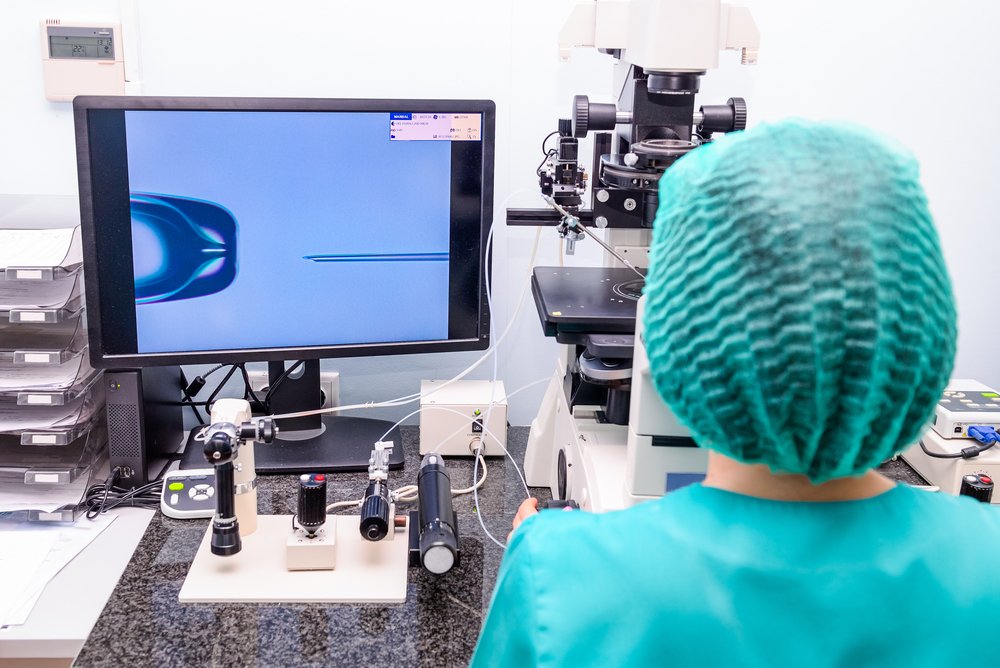
| What it entails | During IUI, sperm is placed directly into your uterus, reducing the distance sperm has to travel, hence increasing the chances of the sperm reaching your eggs. | During IVF, your eggs are retrieved through a quick 10-minute procedure, combined with a sperm, and then back into your uterus. |
| Success rate* | 15-20%* | 40-50%* |
| Monitoring | Optional, depending on the use of medication | Always required |
| Medications | Option of natural, oral or injectable medication | Almost always injectable |
| Surgery requiring anaesthesia | No | Yes, for egg retrieval |
| Location of fertilisation | Female’s body | Laboratory |
| Odds of multiples | Risk is managed with close monitoring and low dosages | Risk is nearly eliminated when only one embryo is transferred |
| Chance for more than one pregnancy | No | Yes, if embryos are frozen for future pregnancies |
| Genetic testing | No | Yes |
| Procedure length | Approximately 2 weeks | Approximately 3 weeks for fresh transfers (embryos can be frozen for months or years) |
| Donor egg option** | No** | Yes** |
| Donor sperm option** | Yes** | Yes** |
*Numbers stated are international success rates and highly depend on factors like age, lifestyle and your type of fertility issue.
**Eligibility to use donor eggs and donor sperm depends on the patient and must adhere to MOH guidelines. Please speak to your doctor to discuss your candidacy.
IUI vs. IVF Cost
The cost of an IUI is significantly less on a per-cycle basis. Furthermore, most successful IUIs happen in the first three cycles. Here’s a breakdown of the usual costs involved in both treatments
| Component | IUI cost | IVF cost |
| Base treatment | $1,000 – $1,500 | $12,000 – $15,000 |
| Medications | $2,000 – $3,000 | $3,000 – $5,000 |
| Doctor consultations | $1,000 – $1,500 | $1,000 – $1,500 |
IUI vs. IVF risks
IUI also poses less risk compared to IVF. Here are a few differences to be aware of:
| Ovarian hyperstimulation syndrome | IUI | IVF |
| Multiples | By transferring only one embryo, the risk is nearly eliminated. | By transferring only one embryo, the risk is nearly eliminated. |
| Ovarian hyperstimulation syndrome | A potential side effect with injectable medications. This is rare in IUI due to lower doses. | More common due to large doses of injectable medications. This has to be managed with antagonist protocol, a high-protein diet, and possibly, acupuncture. |
| Ectopic pregnancy | No additional risk. | 2-5% risk. Ectopic pregnancies occur in 1-2% of unassisted conceptions. |
| Birth defects | No additional effects without medications. Very slight risk with medications. | While evidence remains conclusive, there might be a 1-2% increase in risk compared to unassisted conceptions. |
| Egg retrieval complications | No risks | Though rare, bleeding and infection are possible. |
| Premature birth | No risk. | There is a slight risk for premature birth and low birth weight. |
| Cancer[2] | No risk. | No risk. |
Should I opt for IUI or IVF first?
While IVF has been shown to produce higher success rates[3], generally, it is recommended to start 3-4 rounds of IUI first. This is because IUI is a lot less costly and less invasive. Many underestimate the cost and toll fertility treatments can take on a woman’s body.
Besides, as someone who’s been carrying out fertility treatments for over 23 years, it’s not as simple as relying on statistics – in order for IUI or IVF to succeed, it depends on the specifics of your body.
For example – how old are you? Do you have an underlying condition that affects fertility? Does your partner smoke?
Generally, IUI may be a good fit for couples with:
- A sperm allergy
- Ovulatory infertility (eg. PCOS)
- Mild male factor infertility
- Ejaculation dysfunction
- Cervical factor infertility
- Unexplained infertility
- The need for donor sperm (eg. single women)
However, I do not recommend IUI as a first-line option for couples with:
- Uterine abnormalities (eg. Severe endometriosis)
- Blocked fallopian tubes
- A history of pelvic infections
- Poor semen analysis results
- Good results from a semen analysis and have been trying for a long time to conceive
IUI or IVF, the fertility journey takes time and commitment
Couples seeking fertility treatment must first be ready to accept the inescapable commitment and challenges. Failed IUI or IVF attempts will cost you financially and emotionally. Therefore, it is crucial to have a strong support system and mental preparedness before beginning your fertility journey.
Fertility treatments are not magic, but they can be dealt with successfully if the right steps are taken, which is why regardless of age, you are encouraged to seek help sooner rather than later.
Dr Yeong Cheng Toh is an IVF specialist with more than 23 years of experience under his belt. With his in-depth expertise on all things PGS (preimplantation genetic screening) and PGT-A* (Preimplantation Genetic Testing for Aneuploidies), he loves helping couples with the most challenging of conditions make their genes come true.
*PGT-A specifically helps:
- Women over the age of 35
- Women who have experienced pregnancy loss
- Women who have experienced chromosomal abnormalities in their pregnancy
- Women who have experienced unsuccessful IVF cycles
- Couples who would like to balance the genders in their family
- Couples challenged by male infertility
References
- https://www.straitstimes.com/singapore/politics/parliament-do-more-to-help-couples-trying-for-a-baby-through-ivf-says-louis-ng
- Kroener, L., Dumesic, D., & Al-Safi, Z. (2017). Use of fertility medications and cancer risk: a review and update. Current opinion in obstetrics & gynaecology, 29(4), 195–201. https://doi.org/10.1097/GCO.0000000000000370
- Goldman, M. B., Thornton, K. L., Ryley, D., Alper, M. M., Fung, J. L., Hornstein, M. D., & Reindollar, R. H. (2014). A randomized clinical trial to determine optimal infertility treatment in older couples: the Forty and Over Treatment Trial (FORT-T). Fertility and sterility, 101(6), 1574–81.e812. https://doi.org/10.1016/j.fertnstert.2014.03.012
